This activity is provided by Med Learning Group.
This activity is supported by an educational grant from Novo Nordisk, Inc.
Copyright © 2023 Med Learning Group. Built by Divigner. All Rights Reserved.
WHAT ARE SOME MEDICAL TERMS I NEED TO KNOW TO UNDERSTAND MY DIAGNOSIS?
It is important to understand common medical terms used to describe diabetes and its complications in order to fully participate in making healthcare decisions. The following is a list of definitions for frequently used medical terms
Albuminuria – higher than normal amounts of a protein called albumin in the urine. This may be a sign of kidney disease
Atherosclerosis – thickening of the walls of the blood vessels and formation of fatty plaques in arteries that block the flow of blood. This condition may limit blood flow to the heart and increase the risk of heart attacks and stroke
Beta cell – a cell in the pancreas that produces insulin
Blood pressure – a measurement of the pressure in the blood vessel with each beat of the heart. Blood pressure readings consist of two numbers; the first number represents your systolic pressure, or the pressure in the arteries when the heart beats and fills the artery with blood. The second number represents diastolic pressure, or the pressure in the arteries when the heart rests between beats
Calorie – a measurement of the amount of energy in food. Fats are high in calories and vegetables are low in calories. Ask your doctor about how many calories you need per day to maintain a healthy weight
Carbohydrate – a type of food that consists of sugars and starches. Carbohydrates are broken down into glucose
Diabetic ketoacidosis (DKA) – severe, untreated hyperglycemia (high blood sugar) that requires immediate emergency medical care. DKA occurs when the body does not produce enough insulin and can lead to coma and death if untreated
Glucagon – a hormone that raises the amount of sugar in the blood. Glucagon is sometimes administered to people who have lost consciousness as a result of severely low blood sugar
Glucose – a simple sugar molecule that is the main source of energy in the body
Glycosylated hemoglobin test (HbA1c) – a blood test that measures your average blood glucose level over the past 3 months
Hyperglycemia – high blood sugar levels
Hypoglycemia – low blood sugar levels
Insulin – a hormone that helps the body use glucose for energy
Insulin resistance – a condition in which the body cannot properly use available insulin. This condition is characteristic of type 2 diabetes
Ketones – a waste product produced when the body burns fat for energy. This happens when the body is not able to use glucose for energy because of a lack of insulin or insulin resistance. A large amount of ketones in your system can lead to diabetic ketoacidosis
Nephropathy – damage to the kidneys. A potential complication of long-term diabetes
Neuropathy – damage to the nerves, especially in the feet, hands, legs, and arms. A potential complication of long-term diabetes
Retinopathy – damage to the small vessels in the retina of the eye. A potential complication of long-term diabetes that can lead to blindness
Triglycerides – a type of fat found in foods and produced by the body. High levels of triglycerides increase your risk of heart disease
Type 1 diabetes – a form of diabetes that occurs when the insulin-producing cells of the pancreas are damaged. People with type 1 diabetes produce little or no insulin. This form of diabetes is also known as juvenile-onset diabetes or insulin-dependent diabetes
Type 2 diabetes – a form of diabetes that occurs when the body becomes resistant to insulin and over time stops producing enough insulin. This form of diabetes is also known as adult-onset diabetes or non-insulin-dependent diabetes
Resource:
Resources
Hypoglycemia is a term used to describe low blood sugar readings. A blood glucose reading below 70 mg/dL is defined as hypoglycemia and a reading below 54 mg/dL is severe hypoglycemia. You and your healthcare provider should have a detailed conversation about your specific blood glucose targets to minimize your risk of hypoglycemia. It is important that you are able to recognize the signs and symptoms of hypoglycemia so that you can immediately correct your blood glucose levels. Some of the signs and symptoms of hypoglycemia are listed in the table below. Please keep in mind that different people may experience symptoms differently; however, it is important to recognize the most common ones.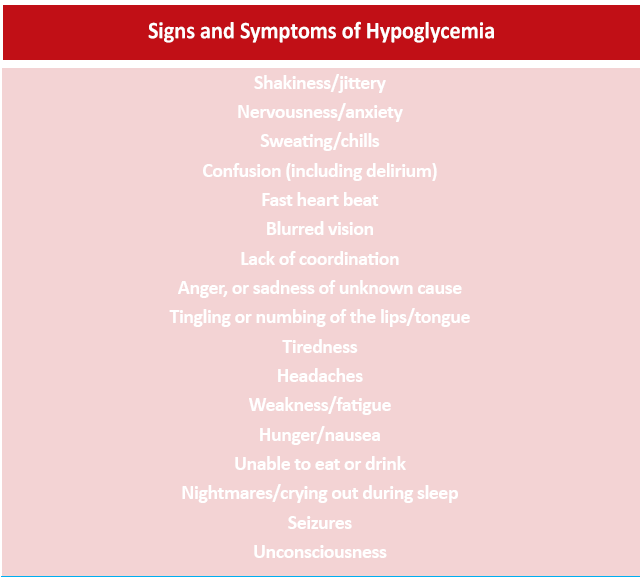
Hypoglycemia can be a side effect of insulin or other types of medications used to treat diabetes. Sulfonylureas and meglitinides are two types of diabetes medications that can cause hypoglycemia. Other causes of hypoglycemia include:
References
In order to treat hypoglycemia, you must quickly raise your blood sugar levels. The best way to do that is to use the “15-15 Rule.”
The “15-15 Rule” is simple. Consume 15 grams of carbohydrate to raise your blood glucose and check your level after 15 minutes. If your blood glucose level is still below 70 mg/dL, consume another 15 grams of carbohydrate. Repeat these steps until your blood glucose is at least 70 mg/dL. Once your blood glucose is back to normal, eat a meal or snack to make sure your glucose levels don’t drop again. Do not eat too much or your glucose levels may shoot too high!
Some examples of quick sources of carbohydrate include:
Avoid using complex carbohydrates, such as pasta, or foods that contain fat along with sugar, such as chocolate. These foods can slow the absorption of glucose and should not be used in an emergency.
The “15-15 Rule” applies to adults. Young children usually need less than 15 grams of carbohydrate to increase their blood glucose level. Discuss the amount of sugar your child needs to correct hypoglycemia with your doctor. Infants may need only 6 grams of carbohydrate, toddlers may need 8 grams, and small children may need 10 grams.
Be sure to tell your doctor if you experience an episode of low blood sugar. They may suggest ways to avoid hypoglycemia in the future.
Resources
GLP-1 receptor agonists are a class of drugs that mimic a hormone in the body called GLP-1. This hormone is produced in the gut and helps the pancreas produce more insulin after a meal. These drugs also reduce the liver’s ability to make more glucose and suppress appetite. Some also keep food in the stomach longer so that patients feel full sooner. All of these effects promote healthy blood glucose levels in people with type 2 diabetes. In addition to effectively controlling blood sugar levels, some GLP-1 receptor agonists also decrease the risk of heart disease and stroke in people with type 2 diabetes. Your doctor may prescribe a GLP-1 inhibitor to protect your cardiovascular health even if your HbA1c is at target.
On average, most patients find that their HbA1c levels drop by as much as 0.5%-1.5% when using a GLP-1 receptor agonist. These drugs are injected under the skin either twice a day, once a day, or once a week depending on the particular medication. Because GLP-1 receptor agonists only help the body release insulin after a meal, there is very low risk of hypoglycemia. Overweight or obese patients generally lose an average of 6.5 pounds with GLP-1 receptor agonists.. The most common side effects of this class of drugs are nausea, diarrhea, and abdominal cramps.
Patients with type 2 diabetes have the ability to produce insulin, but their bodies cannot use insulin properly, limiting the amount of fuel (glucose) the cells receive while increasing the amount of glucose in the blood. When this happens, blood glucose readings will be higher than normal, sometimes resulting in the need for drug therapy in addition to lifestyle modifications. Unlike patients with type 1 diabetes, those with type 2 diabetes can use medications that increase the body’s natural production of insulin or sensitize the cells to insulin. However, as the condition gets worse over time, insulin therapy may be needed to control blood glucose levels.
Type 1 diabetes is usually diagnosed in children and young adults and makes up about 5%-10% of people with diabetes.
References:
Quitting smoking is not easy, but there are strategies that will help you achieve your goal to become smoke-free. Some strategies include:
American Cancer Society. How to Quit Smoking or Smokeless Tobacco. https://www.cancer.org/healthy/stay-away-from-tobacco/guide-quitting-smoking.html
The following is a list of questions about type 2 diabetes that you may want to ask your doctor. Remember to write down any additional questions you have about your health and bring them with you to your appointment.
This activity is provided by Med Learning Group.
This activity is supported by an educational grant from Novo Nordisk, Inc.
Copyright © 2023 Med Learning Group. Built by Divigner. All Rights Reserved.